In an era of accelerating medical innovation, artificial intelligence (AI) is no longer just an analytical tool—it has become an active partner in medical decision-making.
Among its most fascinating and controversial applications is AI’s ability to predict the progression of joint diseases, particularly osteoarthritis. This silent condition that gradually erodes the knees often goes undetected until it’s too late—when pain becomes chronic and cartilage is already damaged.
But what if I told you that algorithms can now visualize what your joint will look like a year from now? And even estimate how much it will deteriorate—more accurately than the human eye?
In this article, we dive deep into this revolutionary technology and explore how AI is reshaping predictive medicine and giving patients a chance to act before pain begins.
🦴 Osteoarthritis: The Silent Disease That Eats Away at the Knees
Osteoarthritis is the most common joint disease worldwide. It’s classified as a degenerative condition that affects the cartilage cushioning the ends of bones. According to global health statistics, over 500 million people suffer from osteoarthritis, with more than 60% of them over the age of 50. In Algeria alone, the Ministry of Health estimates that over 2 million people live with chronic joint conditions.
The disease begins with the gradual erosion of cartilage, leading to direct bone-on-bone contact, pain, stiffness, and restricted mobility. It often progresses silently, with no clear symptoms in its early stages—making early diagnosis a major challenge. This is precisely where AI steps in as a potential lifesaver, capable of detecting subtle changes invisible to the human eye and predicting the disease’s trajectory before it worsens.
📌 Read also: AI in Healthcare: Accurate Diagnosis, Personalized Treatment, and the Future of Medicine
🔍 From X-Rays to Algorithms: How AI Sees What Doctors Can’t
Traditionally, doctors rely on X-ray images to assess joint conditions. However, these images are two-dimensional and only reflect the current state of the joint. AI, on the other hand, transforms these images into time-based maps that can predict how a joint will look months or even years into the future. How? Through deep learning algorithms—particularly convolutional neural networks (CNNs)—trained on millions of labeled radiographic images.
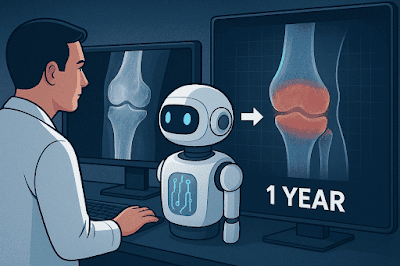
These algorithms don’t just analyze the image; they compare it to disease progression patterns from thousands of other patients. They estimate the likelihood, location, and speed of deterioration. Some models, like the one developed by the University of Surrey, can even generate realistic future images of a joint based solely on its current state. These images feed into predictive systems that calculate a risk index and help doctors make proactive treatment decisions.
A 2024 study showed that this technology achieved 76% accuracy in predicting joint deterioration within one year—compared to just 58% accuracy using traditional human assessment. That’s not just a number—it could mean avoiding surgery or starting preventive therapy at the right time.
🧪 The University of Surrey Study: When Machines Predict Your Joint’s Future
In one of the most groundbreaking studies in medical AI, researchers at the University of Surrey developed a predictive model that analyzes knee X-rays and generates a future image of the joint one year ahead. This model, based on deep learning, was trained on over 10,000 radiographic images categorized by osteoarthritis progression stages.
The results were remarkable:
-
Prediction accuracy reached 75% in moderate cases and 82% in advanced ones.
-
The model accurately identified future erosion zones, helping doctors adjust treatment plans.
-
In 63% of cases, doctors changed their therapeutic decisions after seeing the AI-generated future image.
Most importantly, the system doesn’t just predict—it offers personalized treatment recommendations based on each patient’s unique disease trajectory. In other words, AI doesn’t just tell you what might happen—it guides you on how to prevent it.
🧭 From Prediction to Medical Decision: How AI Reshapes Treatment Plans
In traditional medicine, treatment decisions are based on a patient’s current condition—often as a reaction to symptoms that have already appeared. Predictive medicine, powered by AI, flips this model. Decisions are made based on what “might” happen, fundamentally changing how doctors think.
When a physician sees a future image of a joint showing likely erosion within a year, they can choose a preventive treatment instead of waiting for deterioration.
This shift has tangible benefits:
-
Reduces the need for surgery by up to 30% in early-intervention cases.
-
Improves quality of life through targeted physical therapy designed to slow progression.
-
Cuts long-term healthcare costs, as prevention is far cheaper than late-stage treatment.
In a UK study involving 1,200 patients, doctors altered treatment plans in 63% of cases after reviewing AI predictions. This doesn’t mean machines are taking over—it means they’re becoming strategic partners in care planning.
⚖️ Ethical and Technical Challenges: Can We Trust a Machine to Predict Our Health?
As impressive as this technology is, it raises serious ethical and technical questions. First and foremost: Can we trust a machine’s predictions? Are they accurate enough to base life-changing medical decisions on?
Key challenges include:
-
Privacy: These models rely on sensitive health data like X-rays and medical records. Any breach could have legal and social consequences.
-
Algorithmic bias: If a model is trained on data from one population, it may not perform well on others. For example, models trained on European data may not predict accurately for North African patients.
-
Over-reliance: There’s a risk that doctors may defer too much to AI recommendations, weakening their critical judgment and reducing human interaction in care.
The solution isn’t to reject AI—but to regulate its use, train healthcare professionals to understand its limits, and integrate it into a balanced, human-centered care system.
📈 The Future of Predictive Medicine: Revolution or Passing Trend?
Predictive medicine isn’t a passing trend—it’s a paradigm shift in healthcare philosophy. In the past, medicine treated illness after it appeared. Today, it aims to prevent it before it begins. AI is the engine driving this shift, thanks to its ability to analyze massive datasets and detect patterns invisible to humans.
Models like Delphi-2M, developed by leading AI firms, analyze health records, genetics, and behavioral data to predict over 1,000 diseases across a person’s lifetime. These models don’t just estimate risk—they forecast when a disease is likely to appear, enabling the design of personalized prevention plans.
In the near future, such models may become part of routine checkups—just like measuring blood pressure or glucose levels. But for this vision to materialize, we need robust digital infrastructure, medical community buy-in, and public education on the value of prevention.
🧬 Diseases AI Can Predict and Track Over Time
AI has proven effective in predicting the progression of a wide range of diseases—chronic, genetic, and even psychological. Here are some of the most notable examples:
-
🫁 Lung cancer: CT scan analysis algorithms predict cancer up to 12 months in advance with 94% accuracy.
-
❤️ Heart disease: Retinal image analysis estimates heart attack risk 5–10 years ahead with 80% accuracy.
-
🧓 Alzheimer’s and dementia: Speech and facial movement models predict onset up to 7 years early with 74% accuracy.
-
🩺 Diabetes: Retinal scans detect early signs of diabetic retinopathy and estimate progression speed.
-
🧬 Hereditary cancers: Genetic analysis helps predict breast and ovarian cancer based on inherited mutations.
-
🧠 Delphi-2M: Predicts over 1,000 diseases with 76% short-term and 70% long-term accuracy, estimating onset within ±6 months.
These aren’t just statistics—they’re real tools already in use at research centers and advanced hospitals, forming the backbone of tomorrow’s preventive healthcare.
📌 Read also : 🔥 A Comprehensive Review of the Nvidia DGX Spark: Local AI Like You’ve Never Seen Before
❓ Frequently Asked Questions About AI and Disease Prediction
① Can AI predict diseases before symptoms appear?
Yes. In conditions like Alzheimer’s and lung cancer, predictive models can detect early signals years before traditional diagnosis.
② Are these models currently used in hospitals?
Some are in experimental use at research centers and advanced hospitals. Widespread adoption is limited by cost, regulation, and infrastructure.
③ Can AI predictions be wrong?
Yes. While highly accurate, predictions depend on data quality and may be affected by bias or missing information.
④ Can this technology be used in Algeria or North Africa?
In theory, yes. But practical implementation requires strong digital infrastructure, trained medical staff, and models adapted to local genetic and demographic profiles.
⑤ Will AI replace doctors?
No. AI complements doctors—it doesn’t replace them. Physicians remain the final decision-makers, now supported by predictive insights.
🧩 Conclusion: From Prediction to Prevention… Are We Ready?
AI doesn’t just offer predictions—it offers a rare opportunity: to see our health future before it unfolds, and to act on it. In a world overwhelmed by chronic diseases and strained healthcare systems, predictive medicine is not a luxury—it’s a necessity.
But the real question isn’t whether AI can predict disease. It’s whether we’re ready to listen. Do we have the infrastructure, the medical culture, and the public awareness to turn predictions into prevention?
AI won’t replace doctors. But it will change when they act. And those who act early… win the battle before it begins.